What my turbulent bowel taught me
“Wow, are you hungry or what? Here, take this,” my psychology classmate said while nudging my side with a granola bar. I whispered a polite thanks, barely louder than the rumblings escaping from my lower abdomen. I ditched class during the break and tossed the granola bar in the trash. I wasn’t hungry at all; I was sick.
I was diagnosed with Irritable Bowel Syndrome (IBS) during my sophomore year of college. It’s the medical equivalent of a shrug – doctors acknowledge that a problem exists, but can’t pinpoint an exact diagnosis. While the condition isn’t life-threatening, it isn’t easily cured, either. Most folks who receive this diagnosis struggle to control it for the duration of their lives. IBS encompasses a range of unpleasant symptoms that I’ve struggled to manage for almost ten years. My physical manifestations include extreme bloating, a constant intestinal soundtrack, and frequent bowel movements alternating with constipation. Even after years of experimentation, I have yet to find a definitive cure. I’ve tried a variety of diets, over-the-counter medication, anti-spasmodic prescription pills (bowel muscle relaxers), acupuncture, meditation, herbal remedies. You name it, I’ve done it. Nothing completely works. A food that digests well once could leave me bent over in pain the next time I consume it. Over the course of this search I’ve poured an incredible amount of money and time quite literally down the toilet. My only effective defense against this condition has been behavior modification. As a high schooler, I was an extremely confident extrovert. However, as my symptoms intensified during college, my personality morphed accordingly. I began skipping classes out of sheer embarrassment. My intestines talked more than I did in most courses; it was beyond humiliating because I knew nothing (not even a granola bar) would silence them. The more I thought about them, the worse they seemed to get. I had always been a focused and motivated student, but now spent every class repositioning my body to cope with the bowel brass band playing the song that never ends. I always chose the seat closest to the door or as far away from others as possible. I developed severe social anxiety outside of school. Any quiet social setting was strictly off-limits. Movie nights were excruciating and crowded theaters were even worse. Potluck dinners riddled with digestive landmines were to be avoided at all costs. My digestive tract assumed complete control over my ever-diminishing social calendar and there didn’t seem to be a damn thing I could do about it. I tried to explain my symptoms to friends and family, but many dismissed it or blamed it on poor diet. Their lack of understanding only drove me further towards isolating habits. In particular, dating has been incredibly difficult since my diagnosis. The typical romantic date involves some degree of quiet interaction, but it’s hard to be intimate with a partner when my bowels play third wheel and regularly disrupt conversation. The sound of internal moving parts isn’t exactly an aphrodisiac. I tend to opt for distracting environments when planning a date: a crowded bar over a cozy sushi spot, a noisy concert rather than a movie. While I’d honestly rather get sushi over drinks, see a movie over risking permanent hearing loss, the fact of the matter is that I know better. I know that my body is unpredictable; I know how unattractive my condition is and how difficult it can be to explain. So I plan accordingly.
I’ve even adopted particular habits at work in the office to cope with my symptoms. Every morning, I pop Activated Charcoal supplements followed by Peppermint tea and hope for the best. I spend part of the day seated, but typically stand after lunch to ease digestive pain. When booking conference rooms, I consistently select the two that have noisy air conditioning units to mask my potential internal audio. I always opt to sit next to the door during meetings in case I need to go sit on the toilet for twenty minutes. When things get really severe, I relocate from my deskmates and banish myself to the far-reaching ends of our office: the lobby couch or rarely used breakroom table. On particularly bad days, I work from home and claim I’ve fallen prey to the flu or common cold yet again. The topic of IBS isn’t the most stimulating conversation to have with my boss. IBS has completely altered my behavior and personality. My self-esteem took a serious nosedive immediately following my diagnosis as I learned to manage my symptoms. None of the physical manifestations of IBS are pleasant to talk about or be around. I hated my body. It was a constant source of embarrassment that rebelled against me frequently and unpredictably. It didn’t matter how much money I threw at it, how many hours of research I spent, or the years that went into meticulously planning and documenting experiments with treatment. My digestive and excretory systems functioned outside my locus of control. I became more strategic and introverted in social situations; all of my plans hinged on my bowels. If they were acting up, I’d flake on gatherings with friends, dates, and professional development opportunities for work. My condition dominated my life—it took a long time to cope with that and regain my sense of self. Dealing with IBS has forced me to better advocate for my needs. If I don’t feel like I’ll enjoy an activity, I take steps to make it more manageable or simply decline the invitation. I talk more about my condition now than I ever have before, and try to raise awareness amongst friends and family. While it is unpleasant, I am finally coming to terms with the fact that it isn’t shameful. The more I communicate my needs to others, the better at ease I feel in situations that used to be torturous. Stress and anxiety can be major triggers of a bad episode for me. To combat this, I eat a balanced diet (no more fads), exercise regularly, and strive to get quality sleep. However, that isn’t always enough. Meditation has been a lifesaver. When I’m feeling stressed, I immediately employ meditation techniques to relax and prevent an episode. This practice also comes in useful when I become frustrated by sudden symptom flare-ups; it offers a way to re-center myself. I remind myself that I’m not defined by my condition. I accept that there are things I can’t control, even within my own body. I am still a person of value (bowels included).

Be kind to your mind
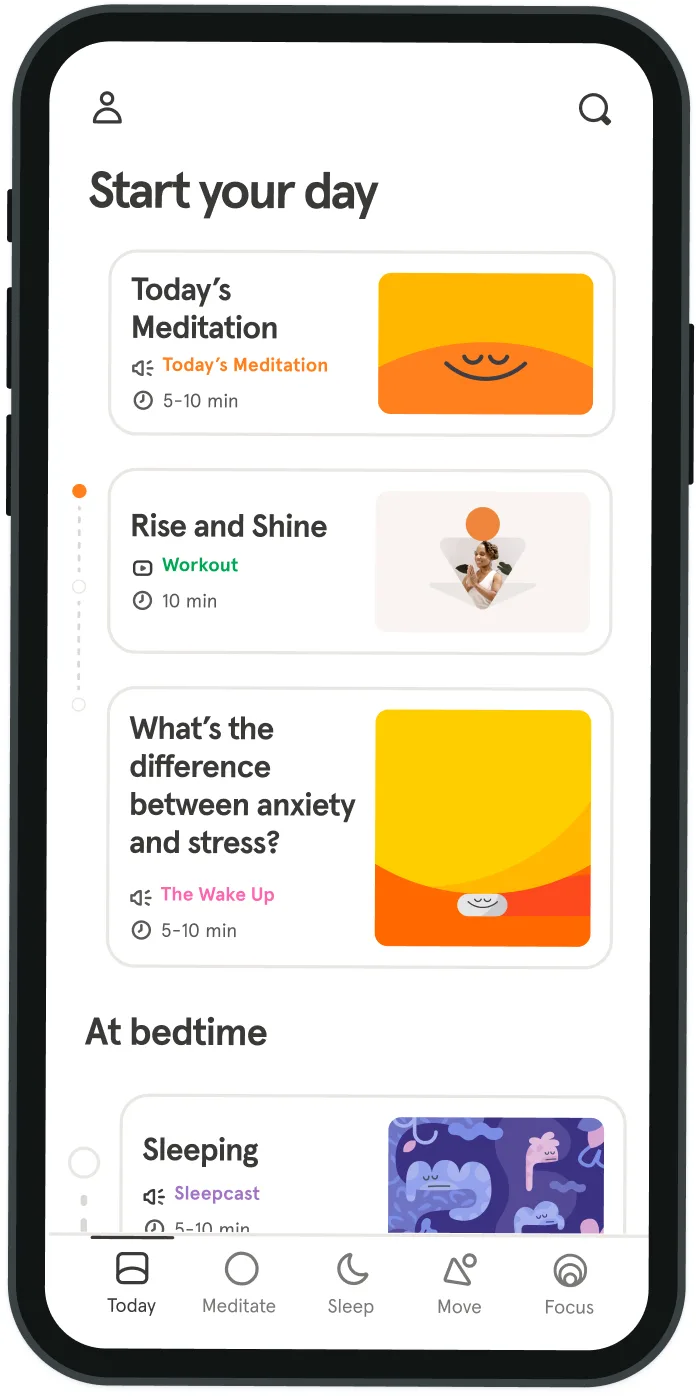
- Access the full library of 500+ meditations on everything from stress, to resilience, to compassion
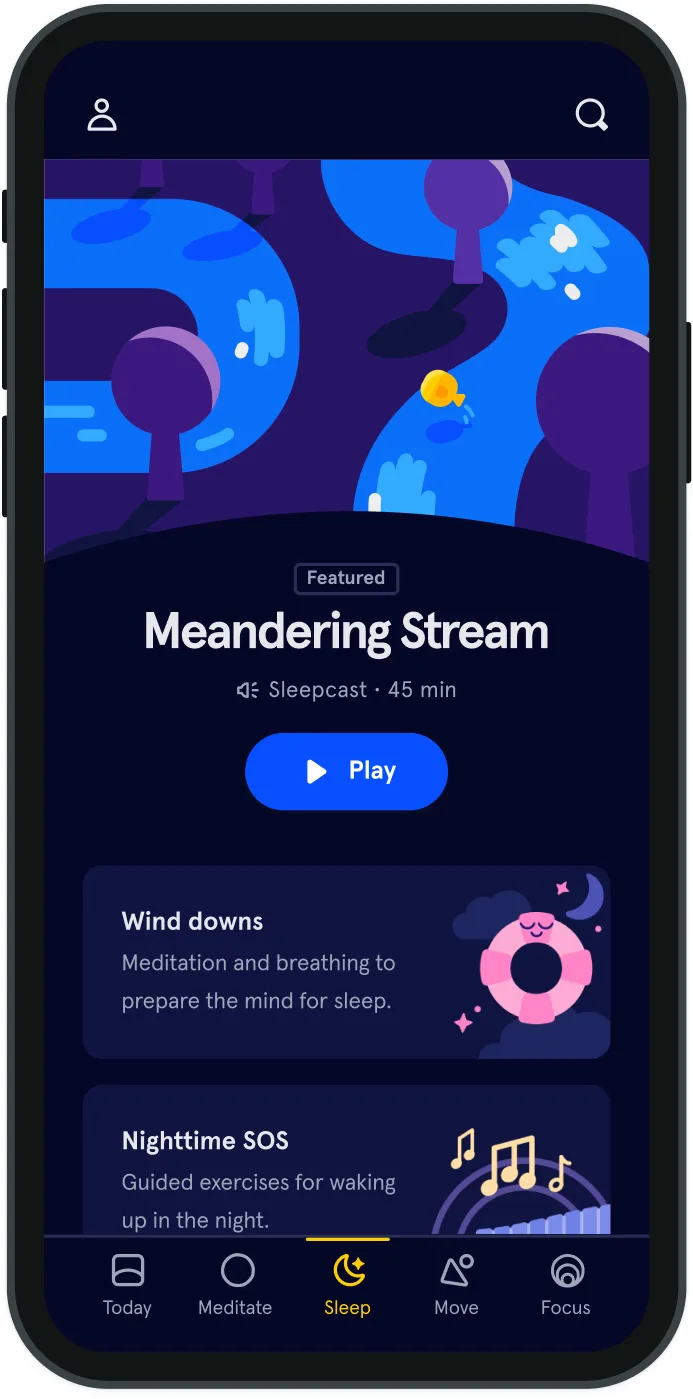
- Put your mind to bed with sleep sounds, music, and wind-down exercises
- Make mindfulness a part of your daily routine with tension-releasing workouts, relaxing yoga, Focus music playlists, and more
Meditation and mindfulness for any mind, any mood, any goal

Stay in the loop
Be the first to get updates on our latest content, special offers, and new features.
By signing up, you’re agreeing to receive marketing emails from Headspace. You can unsubscribe at any time. For more details, check out our Privacy Policy.
- © 2025 Headspace Inc.
- Terms & conditions
- Privacy policy
- Consumer Health Data
- Your privacy choices
- CA Privacy Notice
